TMS FOR MDD
Transcranial Magnetic Stimulation (TMS) is also used to treat Major Depressive Disorder (MDD). In TMS therapy for MDD, magnetic pulses are used to stimulate nerve cells in the brain region responsible for mood regulation. This stimulation is believed to help improve symptoms of depression by regulating brain activity.
TMS for MDD is typically used when other treatments, such as medication and therapy, have not been effective. It is considered a safe and well-tolerated treatment option for depression, with fewer side effects compared to some medications. However, like any medical procedure, there are some risks and potential side effects associated with TMS, such as headaches, scalp discomfort, or, rarely, seizures.
TMS therapy for MDD is usually administered over several sessions, with each session lasting about 20 to 30 minutes. The number of sessions can vary depending on the individual’s response to treatment.
It’s essential to consult with a mental health professional to determine if TMS therapy is a suitable option for treating MDD and to discuss the potential risks and benefits based on your specific situation.
TMS FOR OCD
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure used to treat various mental health conditions, including Obsessive-Compulsive Disorder (OCD). In TMS therapy for OCD, a coil is placed against the scalp near the forehead, and magnetic pulses are delivered to stimulate nerve cells in the brain region involved in OCD symptoms.
TMS for OCD is typically used when other treatments, such as medication and therapy, have not been effective. It is considered a safe and well-tolerated treatment option for OCD, with fewer side effects compared to some medications. However, like any medical procedure, there are some risks and potential side effects associated with TMS, such as headaches, scalp discomfort, or, rarely, seizures.
TMS therapy for OCD is usually administered over several sessions, with each session lasting about 20 to 30 minutes. The number of sessions can vary depending on the individual’s response to treatment.
It’s essential to consult with a mental health professional to determine if TMS therapy is a suitable option for treating OCD and to discuss the potential risks and benefits based on your specific situation.


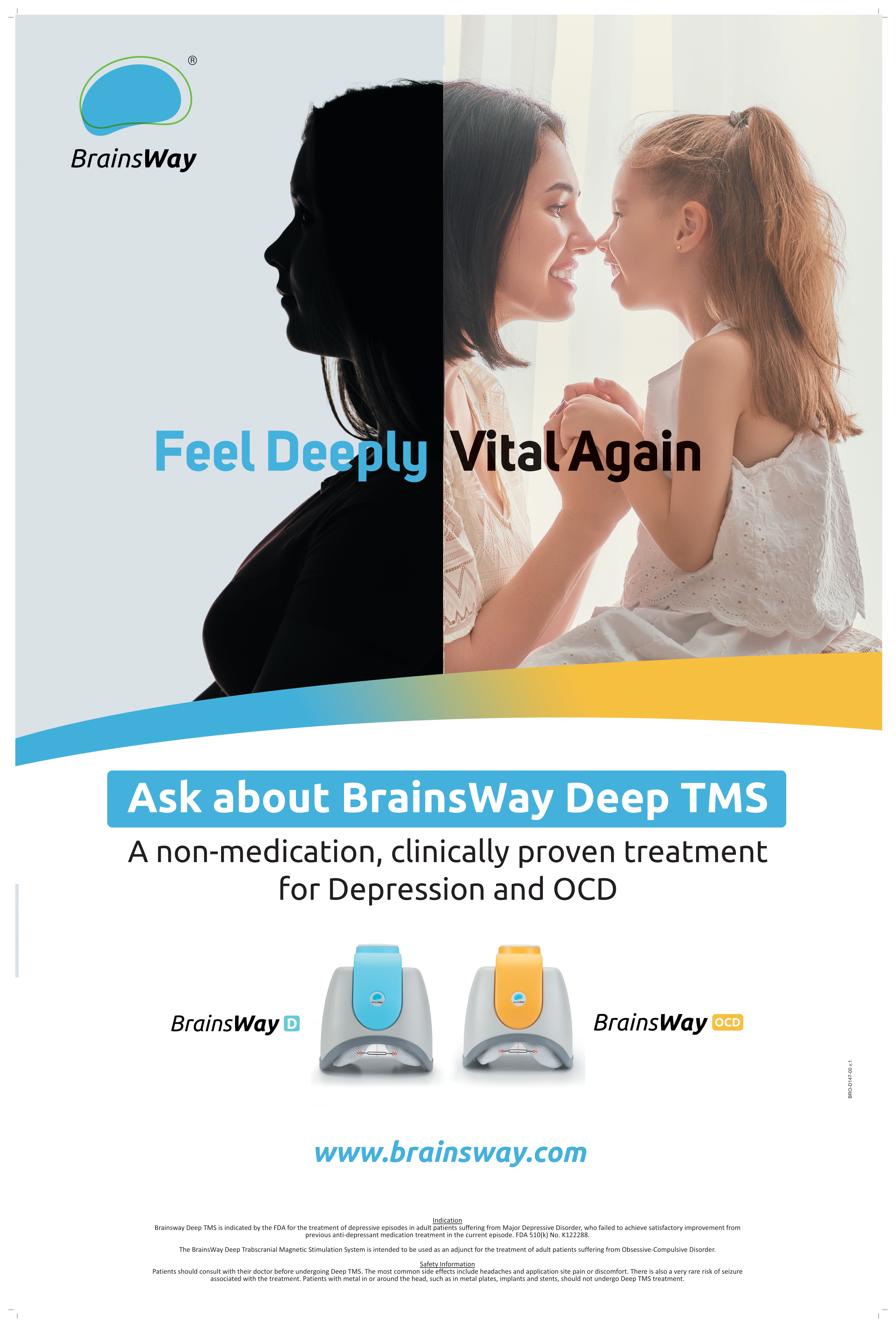
BrainsWay Deep TMSTM Offers Your Patients New Hope for Depression (MDD) and Anxious Depression
What is Deep Transcranial Magnetic Stimulation (Deep TMS)?
BrainsWay Deep TMS is a noninvasive, FDA-cleared, outpatient brain stimulation procedure with proven clinical results for
improving symptoms of depression (including depression with comorbid anxiety).
The technology stimulates neuronal targets using its patented H-Coil, resulting in a deep and broad penetration of the magnetic field into areas of the brain that are affected in neuropsychiatric disorders.
Covered by most insurers for depression, Deep TMS is safe and well-tolerated, has no systemic side effects, and does not require anesthesia.
What Happens During Deep TMS Treatment Sessions?
Each 20-minute session involves stimulation of brain targets with Deep TMS.
The treatment coil delivers gentle electromagnetic pulses to key areas in the brain involved in mood regulation. These pulses feel like mild tapping on the scalp. The patient will be sitting comfortably in a chair, awake and alert during the treatment.
Key points:
• Noninvasive in-office procedure
• No downtime after treatment
• Safe and well-tolerated, with no systemic side effects
• Short 20-min sessions (3-min intermittent theta burst session is also available)
• 20 sessions across 4 weeks followed by periodic maintenance sessions
Why is BrainsWay a Good Option for Your Patients?
Patients with severe depression symptoms do not always respond sufficiently to psychotherapy or pharmacotherapy.
• Recurrent depression episodes, as well as negative expectations about depression treatment, have been shown to be associated
with reduced outcomes for psychotherapy.1, 2
• As shown in the STAR*D study, 63% of depressed patients fail to achieve remission with first-line medication. 33% fail to achieve
remission from any medication treatment.3
Patients often discontinue medication due to serious side effects.
• Antidepressant medication frequently produces debilitating side effects, such as weight gain, sexual dysfunction, suicidal
thoughts, nausea, insomnia, and anxiety.
How Effective is Deep TMS in Treating Depression and Anxious Depression?
Safety and efficacy of BrainsWay’s Deep TMS H1 Coil in alleviating depression symptoms has repeatedly been demonstrated in
multiple clinical studies and real clinical usage.

BrainsWay Deep TMS Indication
BrainsWay Deep TMS is indicated by the FDA for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from MDD and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode. FDA 510(k) No. K122288.
Safety Information—Patients should consult with their doctor before undergoing Deep TMS. The most common side-effects include headaches and application site pain or discomfort. There is also a very rare risk of seizure associated with the treatment. Patients with metal in or around the head, such as in metal plates, implants, and stents, should not undergo Deep TMS treatment.
1 Carter, J.D., et al Patient predictors of response to cognitive behavior therapy and interpersonal psychotherapy in a randomized clinical trial for depression. Journal of Affective Disorders. 128 (2011) 252-261.
2 Carter, J.D., et al Patient predictors of response to cognitive behavior therapy and schema therapy for depression. Australian & New Zealand. Journal of Psychiatry. 52 (2018) 887·897
3 Rush AJ, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report Am J Psychiatry. 163 (2006) 1905-17
4 Igor Filipčić, et al. Efficacy of repetitive transcranial magnetic stimulation using a figure-8-coil or an H1-Coil in treatment of major depressive disorder. J Psychiatry Res. 2019 Jul; 114:113-119
5 SA Harvey, et al. Deep TMS for Major Depression, Interim Post-Marketing Analysis of 1040 Patients. Brain Stimulation 13 (2020) 1842e1862
6 G.Pell, et.al. Efficacy of Deep TMS with the H1 Coil for Anxious Depression. J Clin Med. 2022 Feb 15;11(4):1015









